Shingles: the hidden risk for adults with certain chronic health conditions – closing the health awareness gap


This research is commissioned by GSK (GlaxoSmithKline).
Shingles: a dormant virus waiting within
Shingles is an infection caused by the varicella-zoster virus (VZV), the same virus that causes chickenpox 1. Most adults will have had chickenpox at some point in their lives, unaware that the same virus remains dormant in the body and can reactivate later in life to cause shingles.1,2,3
Worldwide, 1 in 3 adults will develop shingles in their lifetime 1,4,5,6,7 – age, stress, treatment, and disease can lower the strength of the immune system response, increasing the risk of developing shingles.1,2,3,8 9
Yet, understanding and awareness of the link between lower immunity and shingles reactivation is not often clear – particularly in adults aged 50 and over, already living with certain chronic health conditions.
Shingles Action Week 2026: global survey
A global survey, 10 commissioned and funded by GSK, highlights widespread gaps in understanding the risk posed by shingles to adults aged 50 and over living with certain chronic health conditions – highlighting the need for more informed, frequent and proactive conversations among patients and healthcare professionals (HCP) about shingles during health appointments.
The survey asked 6,103 adults living in 10 countries about their perceptions of shingles, its risks, severity and the impact it can have on daily life. All respondents were adults living with at least one of the following chronic health conditions: cardiovascular disease (CVD), chronic kidney disease (CKD), diabetes (type 1 or type 2), chronic obstructive pulmonary disease (COPD), asthma or other immunocompromising chronic conditions.
As Shingles Action Week (23 February – 1 March 2026) shines a spotlight on the pain and disruption shingles can cause, the survey insights reveal a disconnect between knowledge, concern and action, particularly among adults aged 50 and over living with certain chronic health conditions.
“Shingles is often overlooked in health discussions, despite the significant additional burden it can place on adults aged 50 and over who are already living with a chronic health condition such as heart disease, diabetes or kidney disease. People living with certain chronic conditions are at greater risk of shingles, yet there is little action to ensure shingles is addressed as part of more proactive, disease management. Shingles Action Week is an important opportunity to encourage more informed conversations about shingles, as a central strategy to support healthy ageing, ensuring all can live longer and healthier lives.” said Katrina Bouzanis, Director, Policy and Advocacy, IFA.
Risk awareness gaps: perceptions and understanding of shingles risk
When asked about their general awareness of shingles and its risks, more than two in five (44%) respondents had an average understanding of shingles, while over a quarter (29%) knew little or nothing about the condition, its symptoms or related complications.10
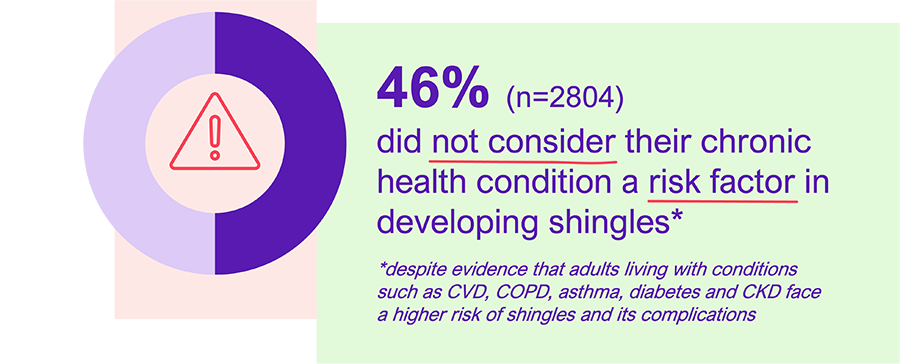
Almost half (46%) of those surveyed said that they did not consider their chronic health condition a risk factor in developing shingles, despite evidence that adults living with conditions such as CVD, COPD, asthma, diabetes or CKD face a higher risk of shingles and its complications.1,9,11,12,13,14,15,16
Respondents living with CVD (47%), diabetes (40%) or COPD/asthma (35%) had the least amount of awareness.10
Importantly, one in four (25%) believe that their chronic health condition does not impact their immune system nor their risk of shingles, and over a third (35%) hold the belief that because their chronic health condition is well managed, they are not at increased risk for shingles.10
“People living with certain underlying conditions may not be fully aware that they are at increased risk of shingles. As immunity naturally declines with age, some conditions, such as diabetes and kidney disease, can further affect immune function. Other conditions, including heart disease, have also been associated with a higher risk of developing shingles. Recognising these risk factors is an important step in prioritising shingles as part of the healthy ageing conversation.” commented Dr Alexander Liakos, Vice President, Global Medical Affairs at GSK.
“I didn’t expect it to be so serious”: shingles disrupting everyday life
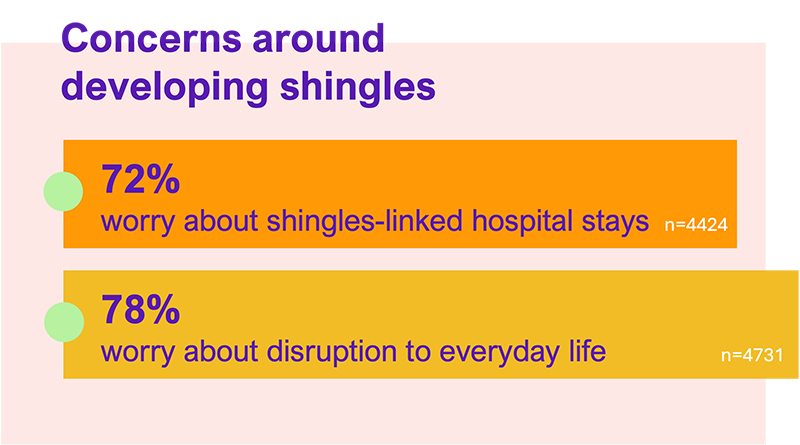
Despite gaps in shingles knowledge and awareness, concerns about shingles potentially disrupting peoples’ lives remain high – a majority (72%) of respondents worry about shingles-linked stays in hospital, and over three quarters (78%) about how it may disrupt their everyday life.10
While concern levels vary by chronic health condition – from 89% among those living with CKD, to 71% among those living with CVD being the most concerned about shingles risk and complications, one in four (25%) of respondents who have had shingles reportedly ‘did not expect [shingles] to be that serious’.10
In fact, 42% reported severe pain that disrupted everyday life, and a third (33%) said shingles stopped them from working or attending social events.10 More so, CKD and COPD patients experienced the greatest disruption, while CKD patients reported the highest emotional impact from shingles.10
“I think there’s still a lot of unawareness and uncertainties about what shingles is all about for a lot of common folks – including myself before I had it! The pain was so excruciating and coupled with the discomfort and the itchiness, it was unbearable, I cannot forget the feeling. I was really feeling scared and lonely.” recalled Mr Lionel Lee, shingles patient, living with CVD.

Limited discussion of shingles risk in healthcare settings
While over two thirds (68%) of adults aged 50 or over living with certain chronic health conditions see their doctor regularly, shingles remains under-discussed.10 In fact, more than half (54%) of respondents have never discussed shingles with a HCP – with respondents living with CVD (53%) and diabetes (51%) being the least likely to have discussed it.10
When asked what would prompt them to enquire about shingles, many respondents highlighted how learning about shingles from a doctor (45%) or an acquaintance who had shingles (37%) was essential to start more informed health conversations about shingles.10
- Many living with COPD/asthma (47%), CKD/CVD (46%), or diabetes (44%) highlighted that personal connection sparks action.10
- Many respondents living with CKD (53%), COPD/asthma (45%), CVD (46%), or diabetes (45%) felt they would especially be responsive to doctor-led prompts.10
Learning about how shingles may impact their chronic health condition management was also highlighted as key prompt for many (43%), while online searches were mentioned only by a quarter (22%).10
A renewed call to prioritise shingles awareness in certain chronic health management
The findings from GSK’s global survey reveal the need for stronger awareness and education around shingles, particularly for adults aged 50 and over living with certain chronic health conditions, including CVD, COPD, asthma, diabetes or CKD. Despite regular interactions with HCPs, discussion of shingles remains limited and many remain unaware that they are at an increased risk of shingles and its complications.
This disconnect, between risk and awareness, emphasises the importance of proactive, informed discussions about shingles as part of routine health management and healthy ageing conversations. HCPs play a pivotal role in bridging this gap, by integrating shingles risk assessments and prevention strategies into standard care for people living with certain chronic health conditions.
This Shingles Action Week 2026, the call is clear: empowering adults with knowledge about their immune health; and encouraging open dialogue with HCPs can help prevent the pain, disruption, and long-term impact of shingles.1,17,18
References
[1] Harpaz, R., et al. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57(Rr-5):1-30; .
[2] Johnson, R.W., et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Therapeutic advances in vaccines. 2015;3(4):109-20.
[3] Mueller, N.H., et al. Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency. Neurologic clinics. 2008;26(3):675-97
[4] Shingles in Australia. Australian Institute of Health and Welfare [Available from: https://www.aihw.gov.au/getmedia/759199ff-f5c8-421d-a572-aaa984a02b49/aihw-phe-236_shingles.pdf.aspx Last Accessed: November 2025]
[5] Curran, D., et al. Meta-Regression of Herpes Zoster Incidence Worldwide. Infectious diseases and therapy. 2022;11(1):389-403.
[6] Lee, C., et al. Lifetime risk of herpes zoster in the population of Beijing, China. Public health in practice (Oxford, England). 2023;5:100356.
[7] Curran, D., et al. Healthy ageing: Herpes zoster infection and the role of zoster vaccination. NPJ Vaccines. 2023;8.
[8] Lasserre, A., et al. Herpes zoster: Family history and psychological stress—Case–control study. Journal of Clinical Virology. 2012;55(2):153-7.
[9] Marra, F., et al. Risk Factors for Herpes Zoster Infection: A Meta-Analysis. Open forum infectious diseases. 2020;7.
[10] Human8 on behalf of GSK. Shingles Action Week 2026 Survey (China, Germany, India, France, Canada, Australia, Poland, Austria, Japan, and UAE). Data on file. 2026.
[11] Steinmann et al. Risk factors for herpes zoster infections: a systematic review and meta-analysis unveiling common trends and heterogeneity patterns. Infection. 2024;52(3):1009-1026. doi: 10.1007/s15010-023-02156-y.
[12] Forbes, H.J., et al. Quantification of risk factors for postherpetic neuralgia in herpes zoster patients: A cohort study. Neurology. 2016;87(1):94-102. REF-36671
[13] Mortimer, K.J., et al. Global herpes zoster burden in adults with asthma: a systematic review and meta-analysis. European Respiratory Journal. 2024 64(2): 2400462.
[14] Ishigami, J., et al. Clinical epidemiology of infectious disease among patients with chronic kidney disease. Clin Exp Nephrol;2019;23:437–447
[15] Kato, S., et al. Aspects of Immune Dysfunction in End-stage Renal disease. Clin J Am Soc Nephrol;2008;3;1526–1533
[16] Okamoto, S., et al. Comparison of Varicella-Zoster Virus-Specific Immunity of Patients with Diabetes Mellitus and Healthy individuals. The Journal of Infectious Diseases;2009;200;1606-1610.
[17] Volpi, A. Severe complications of herpes zoster. Herpes. 2007;14 Suppl 2:35-9.
[18] Kawai, K., et al. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ open. 2014;4(6).